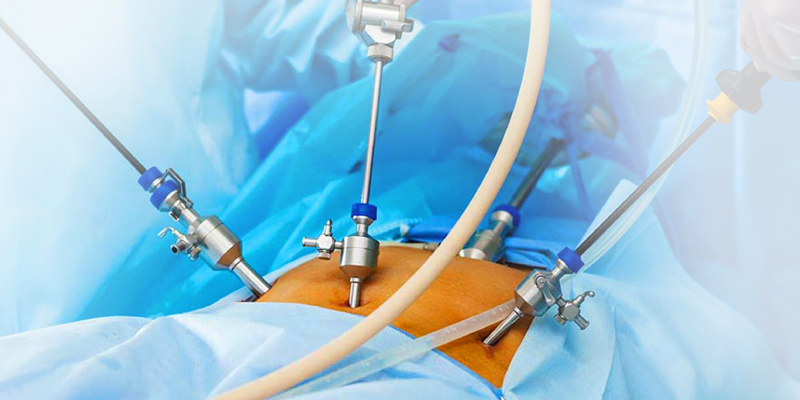
During a pelvic laparoscopy, the expert doctor at Nimai's Borneo Mother and Child Hospitals will use a special tool called a laparoscope to examine your reproductive organs. The laparoscope is a slender tube equipped with a bright light and a high-resolution camera. The laparoscope is pushed through an incision in your abdominal wall. The camera relays images that are projected onto a video monitor. Your reproductive organs can be examined without performing open surgery. Pelvic laparoscopy can also be used to obtain a biopsy and treat some pelvic conditions.
Pelvic laparoscopy is called a minimally invasive procedure because only small incisions are made. Minimally invasive procedures often have a shorter recovery period, less blood loss, and lower levels of post-surgical pain than open surgery.
Doctors at Nimai's Borneo Mother and Child Hospitals use many imaging techniques to observe pelvic abnormalities. These techniques include ultrasound, CT scan, MRI. The doctor may use a pelvic laparoscopy after other noninvasive options have been used. The procedure may be able to provide more detail when the data gathered through these other methods cannot provide a definite diagnosis.
Pelvic laparoscopy can be used to investigate and treat conditions affecting the following organs:
A biopsy of the abnormal tissue is taken during a pelvic laparoscopy. They can also use the procedure to diagnose and treat specific conditions.
You usually will prepare for a laparoscopy in much the same way that you would for any other surgical procedure.
You should tell our expert about any prescription or over-the-counter medications that you’re taking. He can discuss how these medications should be used before and during the test.
Certain medications could affect the outcome of your laparoscopy.
Tell the consultant if you’re pregnant or think you might be pregnant. This will ensure that your fetus isn’t harmed during the procedure.
You may be requested an additional imaging study, such as an ultrasound, CT scan, or MRI before surgery. The data from that imaging study can help them better understand the abnormality they’re investigating.
The imaging results can also provide your him with a visual guide to your pelvic region, improving effectiveness. You cannot eat or drink anything (including water) for at least eight hours before your laparoscopy. If you smoke, you should try to quit.
A pelvic laparoscopy can be done in a hospital, but it’s usually performed in an outpatient clinic.
Before surgery, you’ll be asked to change into a hospital gown. An intravenous line will be inserted into your hand or arm. You’ll get general anesthesia in most cases. This will allow you to remain in a deep sleep and not feel any pain during the procedure.
In other cases, you’ll get a local anesthetic. This type of anesthesia prevents you from feeling pain in your pelvic area during the procedure. However, it will not put you to sleep. You may feel a pricking or burning sensation when you will be injected local anesthesia into your pelvis. You may still feel pressure from the laparoscope during the procedure, but you shouldn’t feel pain.
A small cut will be made above your navel about one-half inch long once the anesthesia has taken effect. A narrow, tube-like instrument called a “cannula” will be placed into your abdominal cavity to expand the cavity with carbon dioxide. This makes room in that area for work. It also allows for a clearer view.
They’ll then insert the laparoscope through the incision near your navel. Up to four dime-sized cuts will be made closer to your pubic hairline. These cuts allow space for additional cannulas and other tools that will be needed to perform the procedure.
A uterine manipulator may also be inserted through your cervix into your uterus. This will help move the pelvic organs into view. All the instruments and gas will be removed from your body and will close all of your incisions once surgery has been completed. Bandages will be placed over the stitches used to close your incisions.
You’ll need to remain in the outpatient facility or hospital for recovery and observation before you can be released. Doctors and nurses will keep a check on vital signs, including:
The amount of time that you’ll need to stay in the recovery area will vary. It will depend on your overall physical condition, the type of anesthesia that was used, and your body’s reaction to the procedure. In some cases, you may need to remain in the hospital overnight.
You’ll be discharged once the effects of your anesthesia have worn off. However, you won’t be permitted to drive yourself home after the procedure. Have someone accompany you to the procedure, so that they can drive you home.
Medication may be prescribed to relieve the pain. Every person reacts differently to the procedure. Follow the doctor’s discharge instructions about when to resume normal activities, such as going to work and doing physical activities. Your post-surgical instructions will depend on the type of procedure you had.
You’ll be instructed not to lift any heavy objects for about three weeks after the procedure. You can resume your normal diet. You’ll need to return to our expert in about two weeks for a follow-up visit.
Pelvic laparoscopy is considered a surgical procedure. The most common complications are bleeding and infection. However, these risks are minimal. Still, it’s important to be aware of signs of infection.
Contact us if you have any of the following:
A pelvic laparoscopy includes a risk of potential internal damage. The doctor will conduct immediate open surgery if an organ is punctured during the pelvic laparoscopy.
The findings of the pelvic laparoscopy will be analyzed by the experts. If a biopsy was taken, a specialist in disease diagnosis called a “pathologist” will examine it in a laboratory. A pathology report detailing the results will be sent to the doctor.
Normal results of a pelvic laparoscopy indicate that the reproductive organs and any other organs examined are normal in size and appearance. A normal report also documents the absence of cysts, tumors, or other abnormalities in the pelvic area.
The doctor may need to order more laboratory tests and perform more physical exams before they’re able to give you a diagnosis.